Molecular and Cellular Mechanisms of Invasiveness of Tumour Cells
Solid cancer: the new tumour spread endpoint opens novel opportunities
Interview with Jan Brábek regarding his recent invited editorial in British Journal of Cancer.
Could you please brief us on the context of your recent editorial in the British Journal of Cancer?
Jan Brábek: First, we thank Drs Adrian Harris and James Mockridge, editors at the BJC, for accepting our modest contribution. Serendipity finds that the direction of our lab is aligned with, and at the confluence of five trends in solid cancer R&D:
- novel drugs that delay metastasis in prostate cancer,
- the wider recognition of oligometastasis,
- advanced imaging,
- the therapeutic potential of precision radiotherapy in early cancer, and
- the recent regulatory guidance on a metastasis-free survival (M-FS) endpoint in clinical trials.
Our short editorial captures the consequences of this change in direction: Solid cancer: the new tumor spread endpoint opens novel opportunities. The current record of pharmaceutical companies R&D in solid cancer is dismal. Although several new drugs have been approved, the extension of meaningful life is measured in weeks. R&D failure failure can be explained, in part, by the regulatory requirement of fixating on the tumor shrinkage endpoint, rather than tumor spread.
We make two points: drug-induced tumor shrinkage does not imply regression of the cancer, and a delay in metastasis signifies inhibition of the natural history of the disease – tumor spread.
In general, current preclinical models are limited to measurements of tumor size; a decrease in tumor mass for cytotoxics, and inhibition of tumor growth for cytostatics. Candidate drugs that do not have an effect on tumor size in the lab are usually not advanced to the clinic. This is because most clinical trials are based on a tumor shrinkage endpoint.
The term “progression” in progression-free survival (P-FS) refers to an increase in tumor size over time, and not an increase in the number of metastases. Ongoing metastasis, rather than an increase in tumor size, is the key determinant of morbidity and mortality.
The recent clinical trials and regulatory approval of novel androgen receptor inhibitors in delaying metastasis, in patients with nonmetastatic castration-resistant prostate cancer (nmC-RPC), is a welcome event, which has the potential to redirect R&D interest away from tumor shrinkage and P-FS, and towards a delay in metastasis.
The M-FS trial endpoint, rather than P-FS, is the gold standard of efficacy as it is a more logical, meaningful, and credible determinant of overall survival.
M-FS also answers the question of patients: Doctor, has my cancer spread?
What is nmC-RPC?
nmC-RPC is not a distinct and homogenous clinical entity, but a transition state between an indolent isolated cancer and an aggressive phase—metastatic castration-resistant prostatic cancer (mC-RPC). It is characterized by rising levels of prostate-specific antigen, castrate levels of testosterone, and the absence of radiographic evidence of metastatic disease. Here, three novel androgen receptor inhibitors, apalutamide (Erleada, Janssen), enzalutamide (Extandi, Pfizer/Astellas), and darolutamide (Nubeqa, Orion/Bayer HealthCare), have shown a delay in M-FS by about 10 months, compared to about 4 months in controls.
M-FS is the time from randomization to either imaging-detectable distant disease or death. Prompted by the robust trial results, the United States Food & Drug Administration issued a draft guidance titled: ‘Considerations for metastasis-free survival endpoint in clinical trials’.
Could you explain the role of imaging and radiotherapy?
Traditionally, and for the most part, radiotherapy has been limited to advanced and inoperable disease, and as a palliative option. With advances in imaging and hypofractionated stereotactic body radiation therapy (SBRT), and the recognition that oligometastasis in early disease may be curable, this approach may soon be considered a curative front-line intervention in selected patients. Oligometastasis is an early stage of metastasis where involvement is limited to a few sites.
Advanced imaging (68Ga-PSMA-11 PET) has supported SBRT and ENRT (elective nodal radiotherapy) in the management of prostate cancer. Initial reports continue to document better-than-expected outcomes for SBRT in selected patients with a variety of oligometastatic solid cancers. ENRT reduces the number of nodal recurrences when compared to SBRT.
However, outcomes in radiotherapy are different from targeted drugs as dead cells cannot develop resistance.
What do you expect in the future?
In the future, we expect that with advances in drugs and imaging/radiotherapy, the boundaries of M-FS in solid cancer R&D will be extended beyond nmC-RPC to other solid cancers. This will increase treatment options for patients with early disease. The main limitations of current drugs relate to limited efficacy, serious adverse events, and of course financial toxicity. Financial toxicity goes beyond product pricing; it includes off-the-book costs related to the management of serious adverse events.
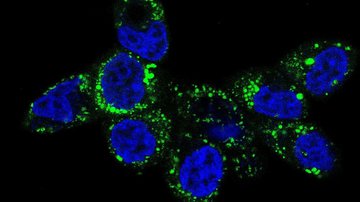
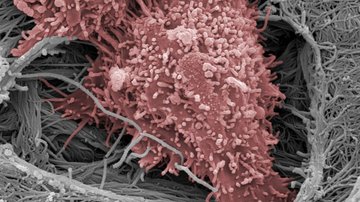
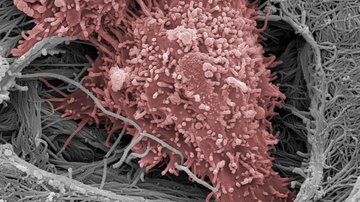
Another aspect we expect improvement is in preventative initiatives, with regards to metastasis, a predictable next-step in early cancer. For a cancer cell to metastasize, it has to move in a deterministic manner and relocate at an optimal site (seed and soil). The common denominator of the migrastatics drug class is to inhibit directional motility. As we have explained, the new endpoint, M-FS, is appropriate for the clinical and regulatory evaluation of candidate migrastatics.
Our program on Migrastatics is directed to the prevention or delay of predictable metastasis, and the recent work at Cancer Research UK on anti-metastatic inhibitors of lysyl oxidase is an important step in this direction.
What is your vision for translational R&D in cancer?
Although much progress has been made in mature therapeutic sectors, translation efforts have not been successful in the absence of a working mechanistic frame, for example, in solid cancer.
Thomas Kuhn advised that innovation demands that dogmas that do not deliver should be questioned. As with the case of the P-FS endpoint, it require debate and possible replacement.
Solid cancer is an exemplar of multi-causal uncertainty, and we look forward to a Big Tent translational approach to replace narrow, disciplinary, and academic silo’s. Membership in this translational tent should be open, and include, for example: cell and mechanobiology, pharmacology, natural products screening, medicinal chemistry, imaging/radiotherapy, epidemiology and public health. Any discipline can take the lead.
But in order to be successful, translational programs requires clinical insight (a balance between efficacy, toxicity, and price), and an understanding of regulatory science.
What would you hope to happen next?
We look forward to academic and industrial partnerships between cell biology, medicinal chemistry, and imaging/radiotherapy which we hope will catalyze a novel, broad-spectrum, and rewarding approach to R&D and the management of cancer. In cancer translational R&D, narrow disciplinary silo’s do not appear fit for purpose.
We also hope for more trial successes as it is the path towards access to valuable medicines that are prescribed for a longer duration, accessible to more patients, priced affordably. Above all, we wish to answer the universal question of patients with solid cancer: ‘Doctor, has my cancer spread ?’
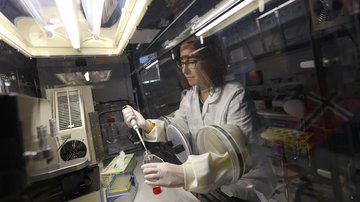
To what do you attribute progress in your laboratory?
First, to our bias towards questions, not answers. Second, to our microenvironment - our enthusiastic colleagues. Third, to our close collaboration with scientists at Charles University and BIOCEV. And finally, to the support we receive from institutional, governmental, and private agencies. Without these elements it would not be possible to contextualize these insights.
Thank you and good luck!
Read the editorial HERE and visit Jan´s LAB
CONTEXT
- Fernandes M, Rosel D, Brábek J. Solid cancer: the new tumour spread endpoint opens novel opportunities. Br J Cancer. 2019; 121: xxx-xxx
- Beaver J, Kluetz P, Pazdur R. Metastasis-Free Survival—a new end point in prostate cancer trials. N Engl J Med. 2018; 378: 2458–2460.
Connell PP, Hellman S. Advances in radiotherapy and implications for the next century: a historical perspective. Cancer Res. 2009;69:383-392. - Hellman S. Karnofsky Memorial Lecture. Natural history of small breast cancer. J Clin Oncol 1994; 12: 2229-2234.
- Tree AC. Editorial. Stereotactic Body Radiotherapy in Metastatic Disease: the known unknowns and the unknown unknowns. Clin Oncol (R Coll Radiol). 2019 Jul 17. pii: S0936-6555(19)30282-1. doi: 10.1016/j.clon.2019.07.002.
- Beaton L, Bandula S, Gaze MN, Sharma RA. How rapid advances in imaging are defining the future of precision radiation oncology. Br J Cancer. 2019;120:779-790.
- Calais J, Ceci F, Eiber M, Hope TA, Hofman MS, Rischpler C, Bach-Gansmo T, Nanni C, Savir-Baruch B, Elashoff D, Grogan T, Dahlbom M, Slavik R, Gartmann J, Nguyen K, Lok V, Jadvar H, Kishan AU, Rettig MB, Reiter RE, Fendler WP, Czernin J. 1⁸F-fluciclovine PET-CT and ⁶⁸Ga-PSMA-11 PET-CT in patients with early biochemical recurrence after prostatectomy: a prospective, single-centre, single-arm, comparative imaging trial. Lancet Oncol. 2019;20:1286-1294.
- Lancia A, Zilli T, Achard V, Dirix P, Everaerts W, Gomez-Iturriaga A, Ingrosso G, Liefhooghe N, Miralbell R, Siva S, Van der Eecken K, Ost P. Oligometastatic prostate cancer: the game is afoot. Cancer Treat Rev. 2019;73:84-90.
- Palma DA, Olson R, Harrow S, Gaede S, Louie AV, Haasbeek C, Mulroy L, Lock M, Rodrigues GB, Yaremko BP, Schellenberg D, Ahmad B, Griffioen G, Senthi S, Swaminath A, Kopek N, Liu M, Moore K, Currie S, Bauman GS, Warner A, Senan S. Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet. 2019;393:2051-2058.
- De Bleser E, Jereczek-Fossa BA, Pasquier D, Zilli T, Van As N, Siva S, Fodor A, Dirix P, Gomez-Iturriaga A, Trippa F, Detti B, Ingrosso G, Triggiani L, Bruni A, Alongi F, Reynders D, De Meerleer G, Surgo A, Loukili K, Miralbell R, Silva P, Chander S, Di Muzio NG, Maranzano E, Francolini G, Lancia A, Tree A, Deantoni CL, Ponti E, Marvaso G, Goetghebeur E, Ost P. Metastasis-directed therapy in treating nodal oligorecurrent prostate cancer: a multi-institutional analysis comparing the outcome and toxicity of stereotactic body radiotherapy and elective nodal radiotherapy. Eur Urol. 2019 Jul 19. pii: S0302-2838(19)30533-0. doi: 10.1016/j.eururo.2019.07.009.
- Koo KC, Dasgupta P. Treatment of oligometastatic hormone-sensitive prostate cancer: a comprehensive review. Yonsei Med J. 2018;59:567-579.
- Patel PH, Palma D, McDonald F, Tree AC. The dandelion dilemma revisited for oligoprogression: treat the whole lawn or weed selectively? Clin Oncol (R Coll Radiol). 2019. pii: S0936-6555(19)30207-9. doi: 10.1016/j.clon.2019.05.015.
- Hellman S. Dogma and inquisition in medicine. Breast cancer as a case study. Cancer. 1993;71:2430-2433.
- Gandalovičová A, Rosel D, Fernandes M, Veselý P, Heneberg P, Čermák V, Petruželka L, Kumar S, Sanz-Moreno V, Brábek J. Migrastatics-Anti-metastatic and Anti-invasion Drugs: promises and challenges. Trends Cancer 2017;3:391-406.
- Nakae K, Yoshimoto Y, Sawa T, Homma Y, Hamada M, Takeuchi T, Imoto M. Migrastatin, a new inhibitor of tumor cell migration from Streptomyces sp. MK929-43F1. Taxonomy, fermentation, isolation and biological activities. J Antibiot (Tokyo). 2000;53:1130-1136.
- Over B, Wetzel S, Grütter C, Nakai Y, Renner S, Rauh D, Waldmann H. Natural-product-derived fragments for fragment-based ligand discovery. Nat Chem. 2013;5:21-28.
- Arai Y, Iinuma H, Ikeda Y, Igarashi M, Hatano M, Kinoshita N, Ukaji T, Simizu S, Umezawa K. Migracins A and B, new inhibitors of cancer cell migration, produced by Streptomyces sp. J Antibiot (Tokyo). 2013;66:225-230.
- Tashiro E, Imoto M. Chemistry and biology of the compounds that modulate cell migration. J Ind Microbiol Biotechnol. 2016;43:213-219.
- Kawada M, Atsumi S, Wada S, Sakamoto S. Novel approaches for identification of anti-tumor drugs and new bioactive compounds. The Journal of Antibiotics 2018; 71: 39-44.
- Laudato S, Aparicio A, Giancotti FG. Clonal evolution and epithelial plasticity in the emergence of AR-independent prostate carcinoma. Trends Cancer 2019; 5: 440-455.
- Chaudhuri PK, Low BC, Lim CT. Mechanobiology of tumor growth. Chem Rev. 2018;118:6499-6515.
- Ladoux B, Mège RM. Mechanobiology of collective cell behaviours. Nat Rev Mol Cell Biol. 2017;18:743-757.
- Voller J, Zahajská L, Plíhalová L, Jeřábková J, Burget D, Pataki AC, Kryštof V, Zatloukal M, Brábek J, Rösel D, Mik V, Tkáč M, Pospíšil T, Gucký T, Doležal K, Strnad M. 6-Substituted purines as ROCK inhibitors with anti-metastatic activity. Bioorg Chem. 2019 Sep;90:103005. doi: 10.1016/j.bioorg.2019.103005.
- Tang H, Leung L, Saturno G, Viros A, Smith D, Di Leva G, Morrison E, Niculescu-Duvaz D, Lopes F, Johnson L, Dhomen N, Springer C, Marais R. Lysyl oxidase drives tumour progression by trapping EGF receptors at the cell surface. Nature Communications 2017; 8:14909.
- Smithen DA, Leung L, Challinor M, Lawrence R, Tang H, Niculescu-Duvaz D, Pearce SP, Mcleary R, Lopes F, Aljarah M, Brown M, Johnson L, Thomson G, Marais R, Springer C. 2-aminomethylene-5-sulfonylthiazole inhibitors of lysyl oxidase (LOX) and LOXL2 show significant efficacy in delaying tumor growth. J Med Chem. 2019 Sep 4. doi: 10.1021/acs.jmedchem.9b01112.
- Brábek J, Fernandes M. Affordable cancer care. Lancet Oncol. 2012;1: 32–33.