Our implant can help treat eye cancer, but we have a long way to go prior to clinical practice, says chemist Širc
A hydrogel implant can help with the treatment of eye cancer, especially in children. It is a new discovery, currently being developed by Czech researchers. “Now we need two or three years to work on it. This will be followed by pre-clinical and clinical testing that can be performed on patients,” says Jakub Širc, a chemist from the Institute of Macromolecular Chemistry CAS / BIOCEV, who outlines the long journey before the new method can find its way into real clinical practice. How far are you with research and development?
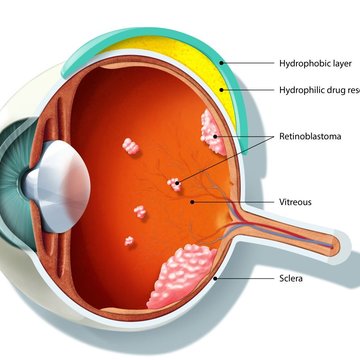
Retinoblastoma is an eye tumour which occurs in children. Until now, if it was caught early, the child would not die but would lose an eye. And you have developed an implant in collaboration with Motol Hospital in Prague that can deliver the necessary substance directly into the eye. Did Motol Hospital approach you, or did you approach them?
It was the result of a discussion in which we talked about all sorts of things; we’ve been working together for a long time. And they came up with the idea that in retinoblastoma, which is the most common malignant, primarily intraocular tumour in children, the problem is to get the drug, the cytostatic, into the eye so that the surrounding organ is not affected...
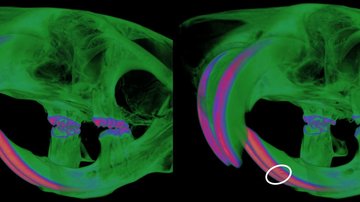
There are two ways to do this: the easiest is via an injection directly into the eye; compared to all other treatments, this is the most gentle one. The second way is an intra-arterial injection, where interventional radiologists insert a catheter through the groin to the blood vessel that supplies the eye and inject the cytostatic drugs there.
This is a super modern way. However, it requires sophisticated instrumentation and interventional radiologists need a lot of practice. And we still have to deal with the downsides. After all, it is a catheter being inserted through the brain, and there’s a risk of bleeding into the brain.
And then there’s a third option...
So how does it work?
It is an implant that resembles a contact lens, but it is made of two layers. The implant is attached to the posterior segment of the eye. The inner layer contains a drug that is gradually released and enters the eyeball, where it attacks the retinoblastoma tumour cells. And then there is an outer impermeable layer that prevents the cytostatic, the drug, from getting into the surrounding blood-permeated tissue and entering the surrounding body.
Does it limit the functioning of the eye?
We’ve performed experiments on rabbits and pigs and this does not seem to be the case. It does not seem to affect the patient’s eyesight. Also, the drugs do not affect the sensitive tissues around the eye and cause irreversible damage.

What all has to happen before you can give the implant to the first patient?
A lot of things. There are three barriers that scientists have to overcome before their inventions can enter into real-world practice. First, it has to be resolved technically, whether in terms of chemistry, physics or medicine, so that it actually works.
The second barrier is legislative, that is, to overcome the boundary between a successful result of applied research and achieving real clinical practice. This means going through legislative barriers that are complicated, but also prevent something that does not work from reaching patients.
And then there is a third barrier, funding. Obtaining funding for specific topics. And that is something that we have not been completely successful with.
So you need a Bill Gates to believe in your idea?
Yes. Now we need two or three years to develop it so that it can go into pre-clinical and then clinical testing which can be performed on patients. And then it could enter real clinical practice.
If I looked into the lab where everything is made, what would I see?
The laboratory for basic and applied research looks similar to the one at a high school. Then there are some sophisticated, relatively expensive instruments that we use to detect cytostatics in various biological matrices. And then there are labs that are used to get the results of applied research into real-world practice. The implants have to be sterile, produced in a sterile environment, that is what clean room laboratories are for.
Source: Lucie Výborná, Prokop Havel (Czech Radio)
Link to the website of the Clean Room Laboratory (IMC CAS in the BIOCEV centre) - HERE